Are you interested in the difference between an EHR and an EMR? This article explains it!
The terms electronic health records (EHR) and electronic medical records (EMR) are used interchangeably. In reality, there’s a significant difference between both systems. This article offers the EHR vs. EMR comparison to clarify the common confusion regarding the terms. You can choose the most appropriate system for your healthcare facility using this information.
EMR Definition
What’s an EMR? Let’s start with its definition. EMR stands for “Electronic Medical Record.” It’s a digital version of a patient’s medical history and current health information, stored and accessible through an electronic database. It involves data about the existing conditions, treatments, and health prospects. The idea behind EMRs is to simplify the work of doctors by allowing them to access traditional patient records via electronic devices. EMR meaning for healthcare is tremendous: it helps organize treatments. The defining feature of an EMR is that it’s present within one hospital. Such records can’t be shared in the majority of the cases.
EHR Definition
What’s an EHR? An Electronic Health Record (EHR) is a digital version of a patient’s medical history and current health information that can be shared across multiple healthcare providers and organizations. The key information includes traditional medical knowledge and data on outside health factors, such as patient demographics and insurance. EHR meaning is simple: its goal is to create a general user profile offering a full-scale insight into patient health. Via it, the doctors can make an overall judgment on the existing lifestyle of the individual and decide what to analyze and treat regarding them.
When Is It Better to Use an EMR vs EHR?
It’s time to perform the EHR vs. EMR comparison. Both frameworks have their positives and negatives. When to use an EHR versus EMR? EHR systems are crucial when you want to share information between multiple hospitals. For instance, if your facility treats a patient with some chronic disease, referring them to various organizations makes sense. A person with chronic pain may need not only medication but also psychological help. An EHR is crucial in such cases because it can provide all the relevant specialists with data on the patient. Knowing about their lifestyle and medical characteristics, these individuals will be able to create efficient treatments. EHRs are essential for treating conditions that have long-term negative impacts and need continuous interventions.
And what about using EMR versus EHR? As we’ve mentioned before, EMRs are the internal hospital records. They contain health-related information vital for a particular facility. When is such a format preferable? It’s good when there’s no need to share the data between multiple facilities. What are those situations? They involve cases of disease necessitating treatment only from one organization. A person with a severe case of flu may need the intervention of one hospital because the disease is non-chronic and doesn’t require any outside specialists. A broken bone is also an example of a condition needing the intervention of one facility. In short, EMRs are crucial for non-chronic diseases. They involve situations in which individuals need only short-term interventions. Their goal is to serve as the data format for spreading information between specialists within one hospital. Demographic information or data on insurance are unnecessary here because the relevant disease may involve no social component, and the person addresses the facility with which they cooperate constantly.
EHR vs. EMR: Advantages
Now that we know the difference between EHR and EMR, it’s time to review the advantages of those frameworks.
Advantages of EHR
An average EHR does several important things for the relevant stakeholders:
- It provides a comprehensive and longitudinal view of patient health information. Using an EHR, it’s possible to see the development of the patient’s health. It’s essentially a ‘curriculum vitae’ for a person’s health status. Via it, one can see the history of a certain condition and even the factors leading to its rise.
- It enhances patient safety and quality of care. The ability to spread information among multiple hospitals is one of the advantages of an EHR vs. an EMR. Let’s imagine a person with chronic pain goes to a psychologist to treat their anxiety and learn how to manage pain psychologically. Without an EHR, the psychotherapist may prescribe anti-anxiety medication conflicting with the other treatments. An EHR helps prevent such medical errors by allowing a comprehensive review of patient information.
- It improves communication and coordination of care among healthcare providers. Certain patients require interventions from multiple specialists. An EHR is a perfect framework for ensuring efficient communication between them. All involved parties can review the records and make their decisions regarding the treatment of a patient. It’s even possible to leave some notes for the other specialists. This factor is a major advantage of EHR vs. EMR.
- It facilitates population health management and public health reporting. EHRs are notable for their ability to boost the overall analysis of health data regarding the population. When multiple hospitals contribute to patient information, the decision-makers can get a comprehensive insight into the condition of a certain individual. Data from many people later enables the analysis of the overall population health. With this information, one can detect some negative trends and later prevent them.
- It enhances research capabilities and supports clinical trials. Another positive of EHR vs. EMR is boosting healthcare research. The data mentioned above not only upgrade public health reporting but also offer insights for clinical trials. Knowing the trends in the population’s health, the decision-makers can choose which diseases need the most focus and find the vital trends in the progress of certain illnesses. This information later allows one to analyze how to proceed with some trials, for example, by highlighting the main trends.
Advantages of EMR
EMRs also have some unique benefits:
- They facilitate quick and easy access to patient health information within a single healthcare organization. EMRs share many advantages of the EHRs. In this regard, they simplify access to information for doctors and patients. What exactly do EMRs do? They enable many smart hypertext features not available in traditional paper records. One can find a patient’s record by typing their name. It’s also possible to perform an internal search within their health records with such frameworks. With such tools, any specialist in a healthcare facility can quickly get important information. This approach saves time and, as the further points will show, improves the accuracy of the frameworks in question.
- They increase the accuracy and completeness of patient records by reducing paper-based documentation. Paper-based documentation has a significant downside: searching for information is difficult. Firstly, those systems require outdated archive frameworks for searching data about patient profiles. Secondly, they’re difficult to navigate due to the written nature of the records. All these problems can lead to the loss of patient data or medical errors stemming from incorrect interpretations. In this light, an investment in Electronic Medical Records makes sense: they improve the accuracy of the doctors involved in patient treatment.
- They boost efficiency and productivity by automating routine tasks such as medication ordering and lab results tracking. Traditional health records require time for analysis to ensure a doctor makes a correct decision regarding the treatment of a patient. With EMRs, one can find vital information, order medication, or track results faster.
- They enable clinical decision support and evidence-based medicine to improve patient outcomes. With EMRs, doctors can use internal statistics tools to track patients’ health data in long-term scenarios. This approach enables evidence-based medicine as one may use the real progress of an individual to make full-scale judgments on their health-related state. It’s also easier to share the data between doctors to enable clinical decision support. In this regard, the difference between EMR and EHR is only in the scope of data sharing. EMRs help share data within one hospital. EHRs are about sharing data in multiple facilities.
EHR vs. EMR: Disadvantages
An EHR vs. EMR comparison also needs to involve some key disadvantages. Here they’re:
EHR Disadvantages
EHR disadvantages are numerous:
- High implementation and maintenance costs. EHRs require one to invest major funds into computer devices and software. To create comprehensive records of the patients, one needs to promote a system working across multiple facilities. An EHR vs. EMR contest is won by the latter framework in terms of price because an EHR requires cooperation from multiple organizations, demanding tremendous long-term costs.
- Significant training and change management requirements. EHRs aren’t easy to control in the majority of cases. These systems require major knowledge on the part of the doctors and other healthcare specialists. One must know how to work with their interface and share the data. Training and change management become essential in those conditions due to discipline-related issues too. One needs to record more data within an EHR rather than EMR. In this light, the “EHR vs. EMR” contest favors the latter framework concerning the simplicity of use.
- Potential disruptions of patient privacy and security if not properly implemented and managed. The problem with all electronic systems is that they’re a potential security liability. Any system connected to the Internet (EHRs need it to transmit data between hospitals) is open to an attack from the outside. Modern tools targeting the prevention of outside interventions exist. Nonetheless, they have a downside: such systems are costly. It’s also crucial to invest in user training as some attacks result from ‘social engineering,’ using human weaknesses (inattention, for instance) to hack well-protected systems. Paper systems may be inconvenient, but they’re impossible to hack due to being non-digital. The EMR vs. EHR contest has an obvious winner again: isolating the EMR systems from outside influences is much easier because they spread information within one hospital.
- Clinician burnout and information overload due to the volume of data captured and displayed. EHRs improve the flow of information and increase the amount of data one can access. Regrettably, this positive turns into a major negative for some professionals. EHRs may lead to information overload. For example, when treating a patient with some chronic illness, the professionals will likely encounter their medical history. It can be confusing and even end in some errors of omission. Modern facilities must invest major funds into information filtering systems to prevent similar situations from happening.
EMR Disadvantages
Here are some disadvantages of EMRs:
- Limited interoperability with other healthcare organizations or providers. EMRs, as mentioned before, are specific to particular hospitals. This information means spreading the data about an individual is difficult in such cases. If there’s a need for outside treatments, this scenario can lead to slowdowns. In this light, the EMR vs. EHR choice is obvious for chronic illnesses: EHRs are superior because they enable treatment in multiple facilities.
- Failure to provide a comprehensive view of a patient’s health if they receive care from multiple providers or organizations. EHRs don’t only prevent interoperability but also limit the amount of information. They contain data relating only to a particular hospital. In this light, such systems don’t give enough information to make full-scale decisions on patient health. The EMR vs. EHR contest is again won by EHRs. EMRs are good for minor episodes of illness but fail at something long-term.
- Potential disruptions of patient privacy and security if not properly implemented and managed. Even though the risk is lower than for EHRs in this case, EMRs are also a problematic technology regarding security due to the practices of modern hospitals. EMRs don’t require access to the Internet and work well within the local networks, minimizing the risks. The problem is that many users still need the Internet on their PCs or laptops. This factor is a major pathway into even the most secure systems: one can first hack an Internet-capable device and then enter the local network. The only solution is to fully isolate EMR computers from the Internet; this approach may require major expenditures on additional computers.
Do Medical Practices Need EHR or EMR Systems?
Medical practices need some electronic records systems. They’re too potent in terms of convenience to ignore them. The choice of EMR vs. EHR should depend on the nature of the conditions one treats. An EMR is perfect when you need more security and work with short-term (even acute) health problems. As for the EHRs, we believe they’re great for long-term conditions needing data sharing between multiple facilities. Nir Menachemi and Taleah H. Collum from the Department of Health Care, Organization, and Policy at the University of Alabama at Birmingham note that electronic records improve long-term patient outcomes. Installing such systems is essential if you want your hospital to succeed.
EMR vs. EHR Implementation: Is it Difficult?
EHR and EMR difference isn’t large regarding the implementation of both systems. EMR and EHR implementation can be complex and challenging, requiring significant planning, resources, and stakeholder engagement to ensure successful adoption. The only difficulty making EHRs slightly more complex is that they work with multiple facilities. Integration between several organizations can be a major barrier. EMRs, however, also have a unique challenge. Due to creating a false sense of security, one must dedicate more time to teaching employees how to avoid major security-related mistakes.
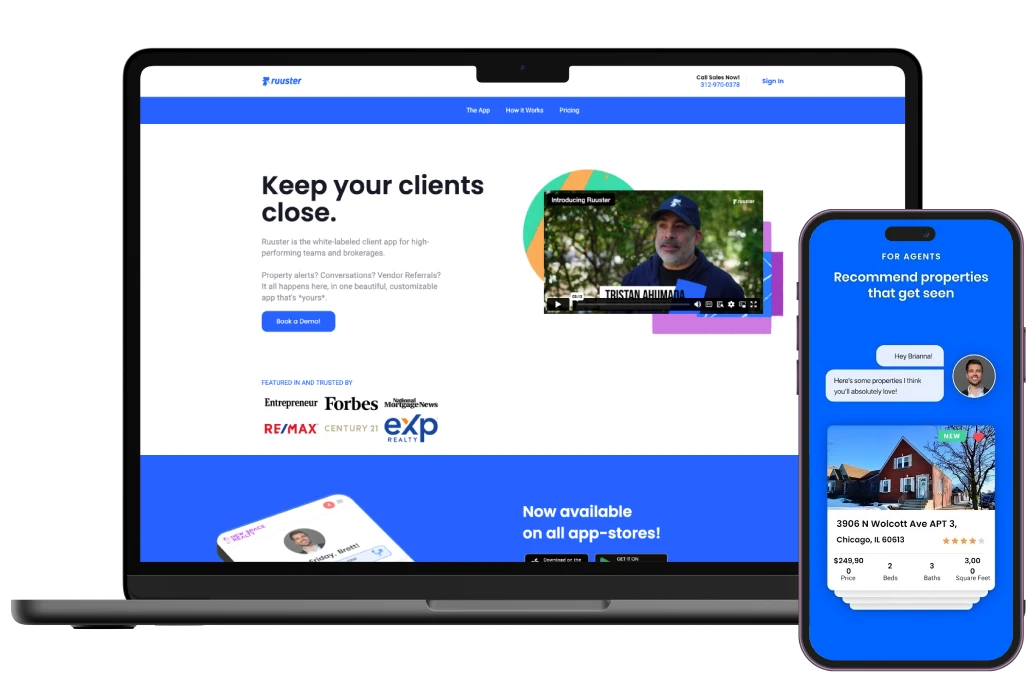
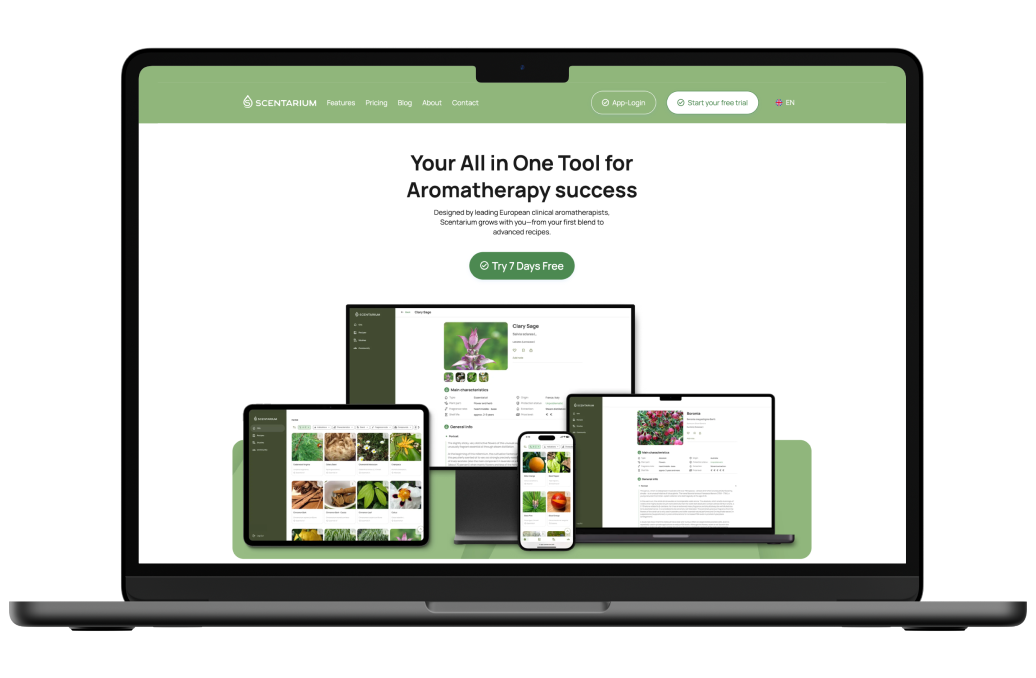
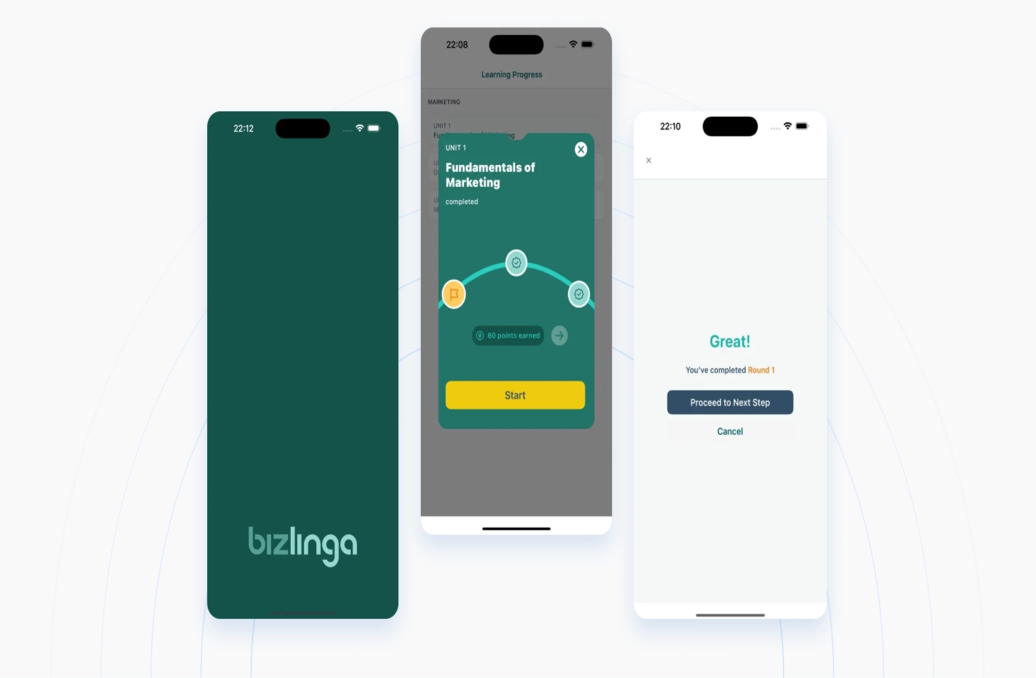
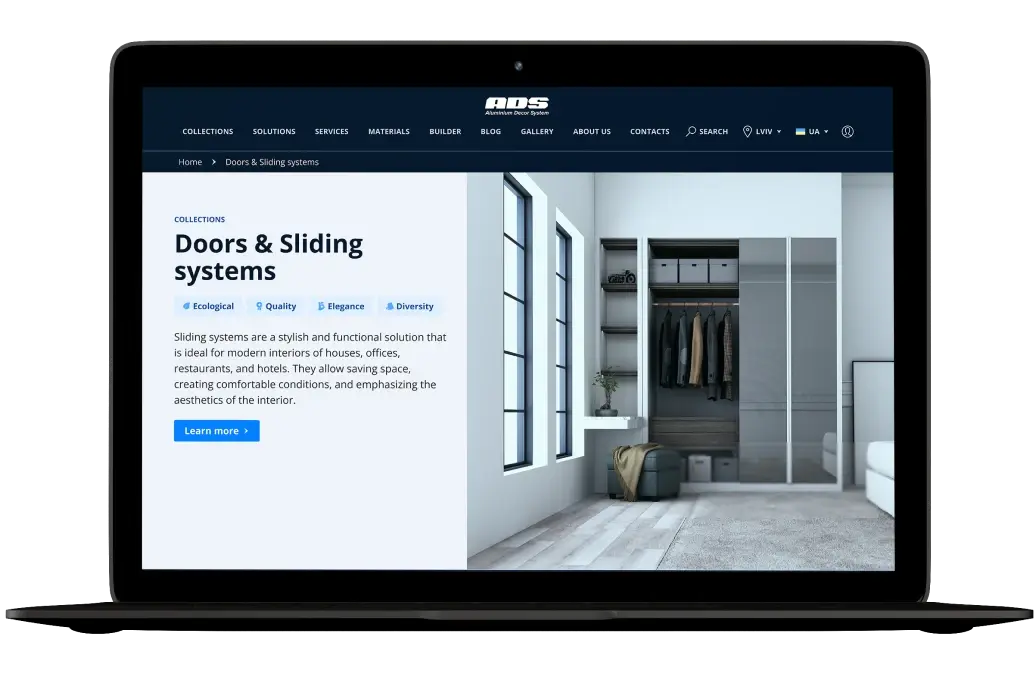
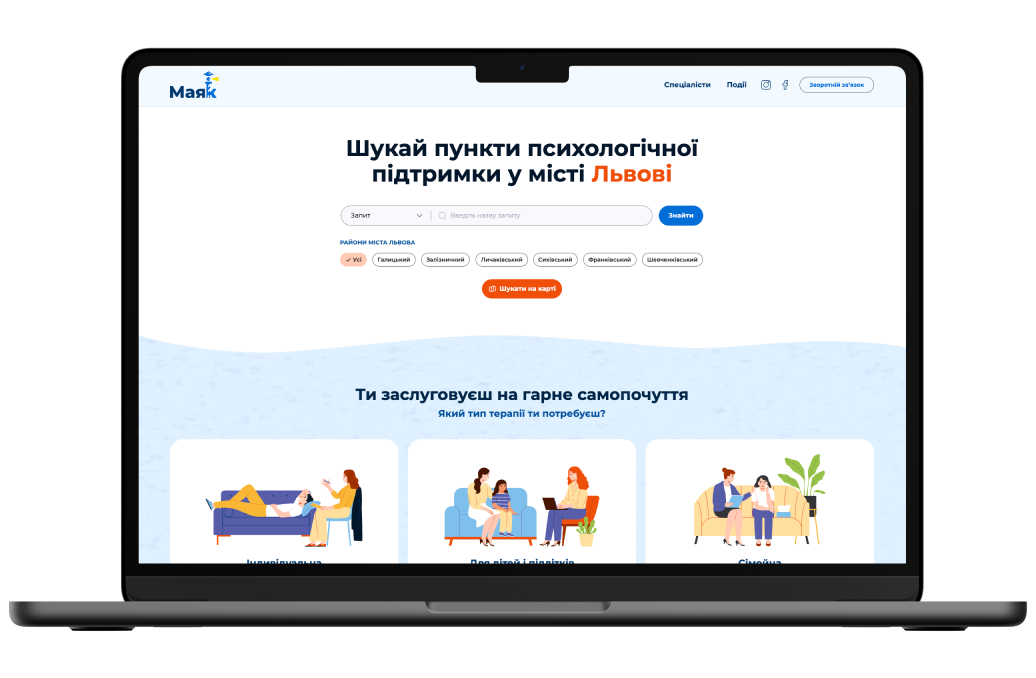
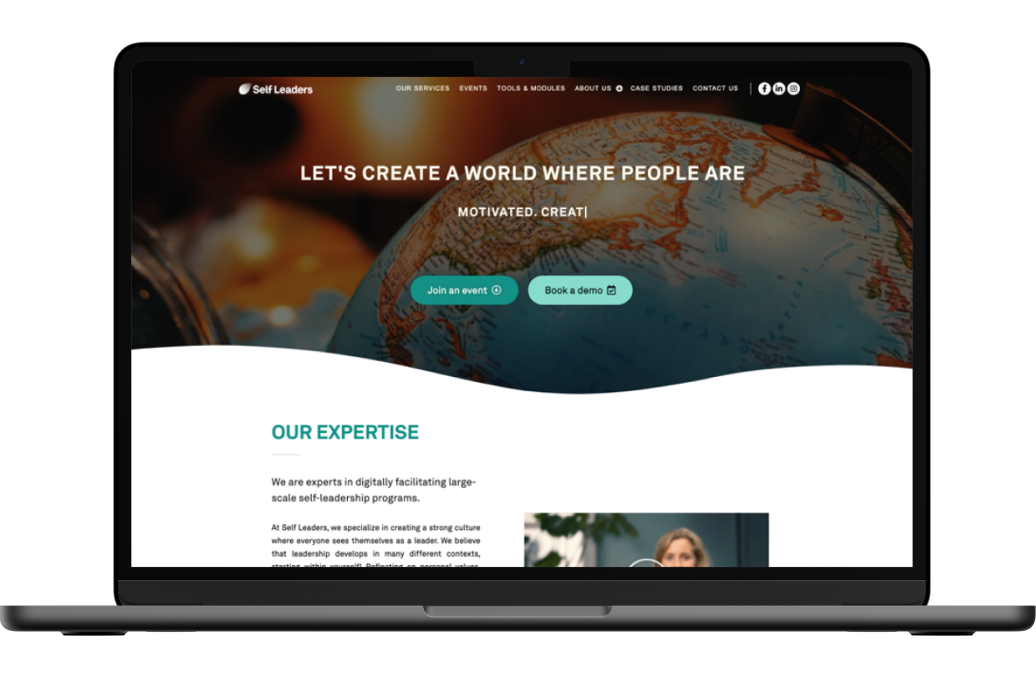
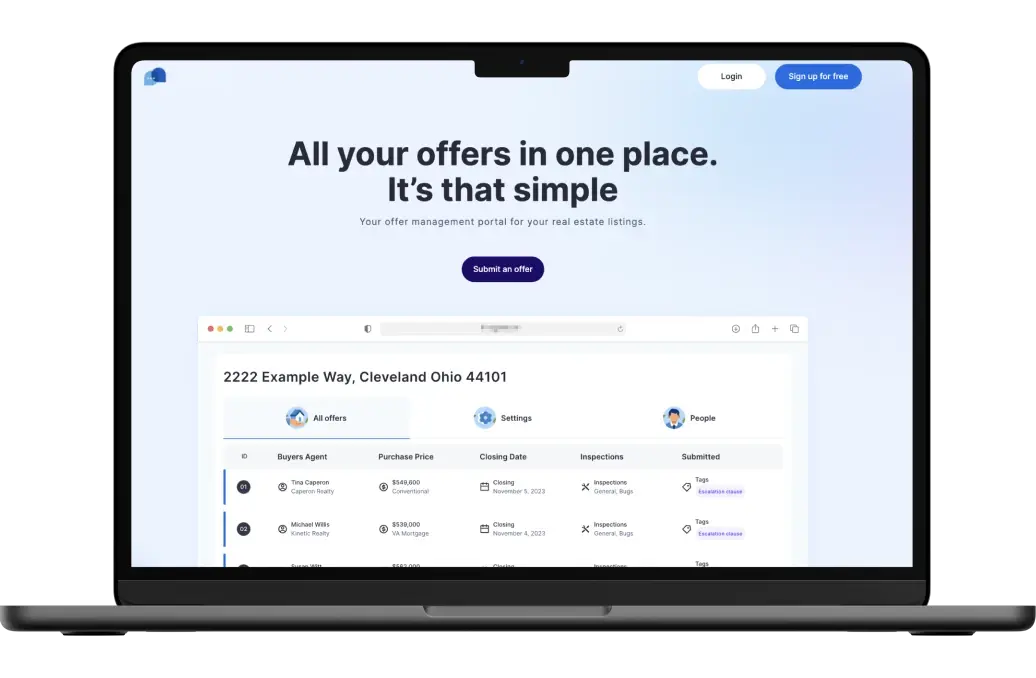
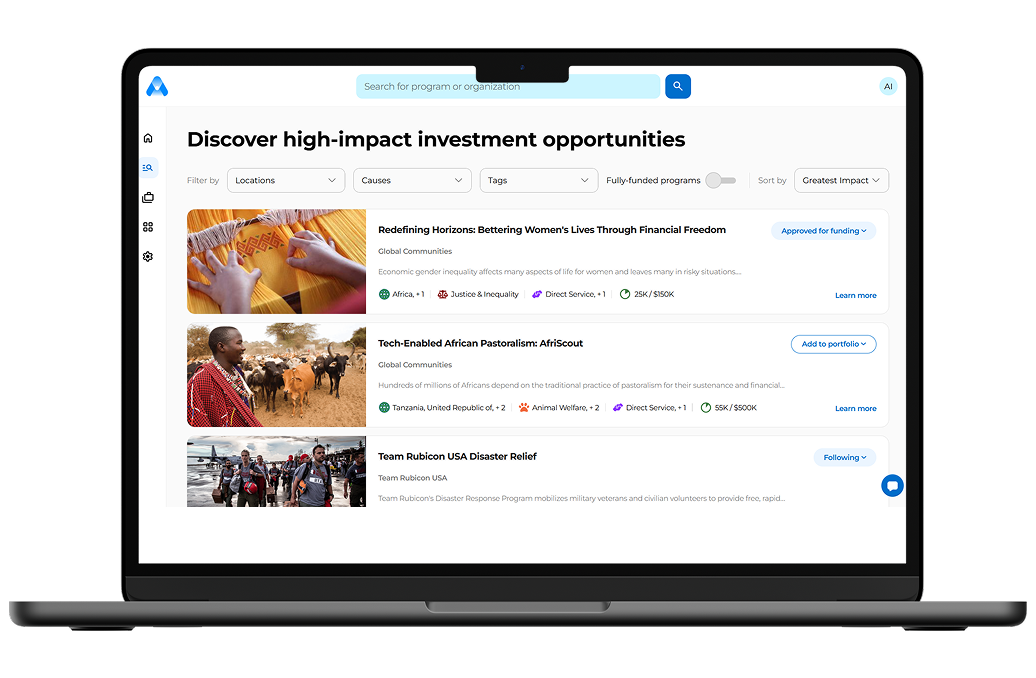
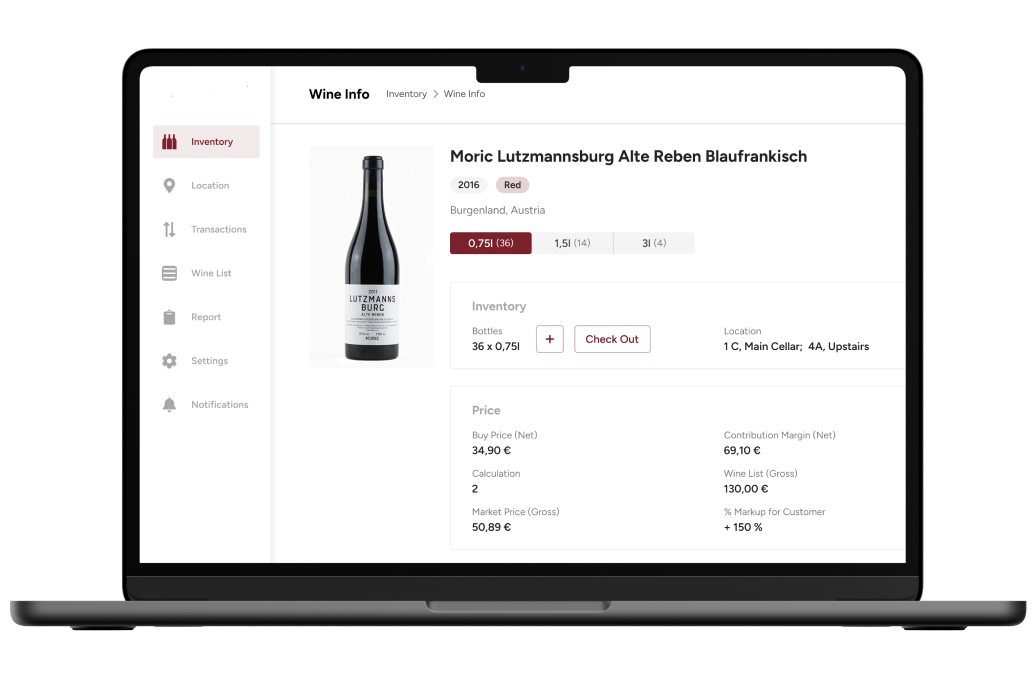
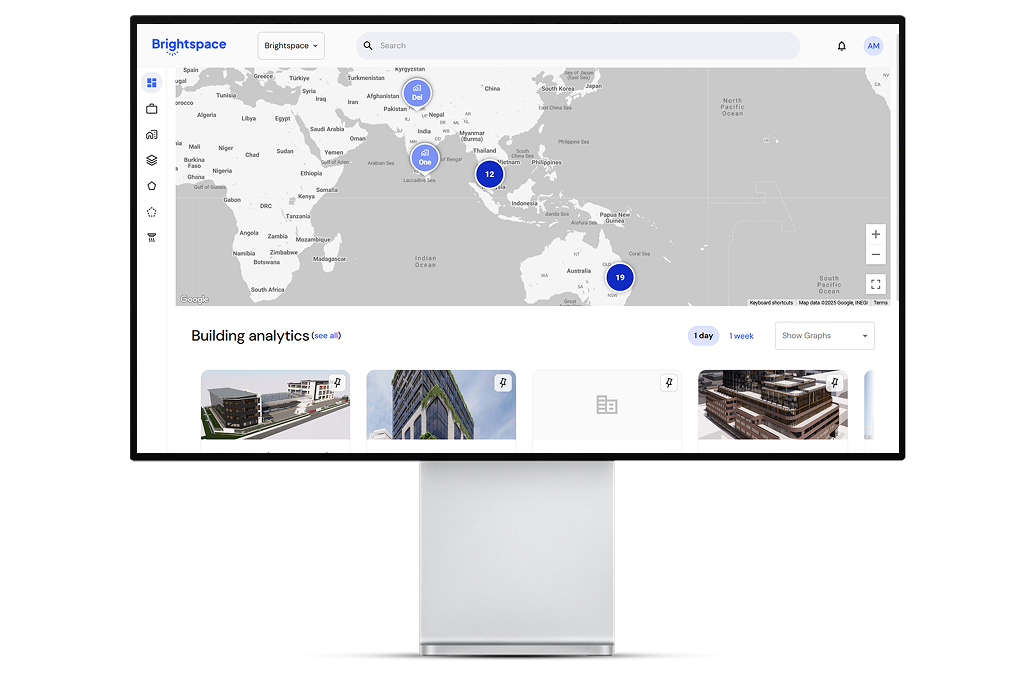
Development of EHR or EMR: Creating Your Software
What software should I choose for an EHR or an EMR? That’s a common question we get. In this respect, you have two solutions. Firstly, it’s possible to choose off-the-shelf apps. They may seem less expensive than custom ones and offer pre-made tools for your hospital. What’s the catch of those systems? They’re inflexible and can feature things you don’t need. Secondly, a great option is to develop custom software. It may be more expensive in the short term but saves money in the long term. Why? The reason is simple: this software belongs to you and targets your unique needs. If you’re interested, our company, Keenethics, provides electronic record development services. We can help you understand the EMR vs. EHR difference and consult on the relevant features. Ultimately, Keenethics’ specialists know how to develop a full-scale product for you. Get a free estimate of the project scope here.
Conclusion
To summarize, the presented information shows investments in EHRs and EMRs are a potent idea. We’ve outlined the benefits and negatives of these frameworks. Using this data, you can make a full-scale decision on developing your systems. If you need any help, don’t hesitate to address our company. Our portfolio features several healthcare-related projects.
Common Questions About the Difference between EHR and EMR
EMR or EHR?
In this case, everything depends on your needs. EHRs are perfect for the management of chronic diseases. EMRs may be great in cases you deal with short-term disorders.
What to look for in an EHR?
When selecting an EHR system, consider its functionality, ease of use, customization options, interoperability, data security, and privacy, vendor support and training, and cost.
What to look for in an EMR?
When selecting an EMR system, consider its functionality, ease of use, customization options, data security, and privacy, vendor support and training, and cost. Interoperability may be less important compared to EHR.
Are EMRs safer than EHRs?
If properly managed, EMRs can be safer due to being isolated from the Internet. However, one needs to invest more funds into hardware to isolate them from the network.
Contact us to start developing a unique solution!